Emergency War Surgery NATO Handbook: Part I: Types of Wounds and Injuries: Chapter III: Burn Injury
Escharotomy
United States Department of Defense
Peer Review Status: Internally Peer Reviewed
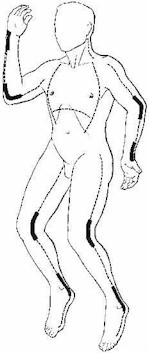
Circumferential full-thickness burns of the limbs may impair the circulation to distal and underlying unburned tissue. To prevent secondary ischemic necrosis of these tissues, an escharotomy may be necessary to relieve constriction caused by edema beneath the inelastic, unyielding eschar. The adequacy of the circulation of a burned limb must be assessed on a scheduled basis, e.g., hourly. The most reliable assessment of the circulation can be made by using an ultrasonic flowmeter to detect pulsatile flow in the distal palmar arch vessels in the upper limb and the pedal vessels in the lower limb. Absence of pulsatile flow or progressive diminution of flow on sequential flowmeter examinations is an indication for escharotomy. If a flowmeter is not available, the caretaker must depend upon the less reliable clinical signs of circulatory compromise. Swelling and coldness of the distal unburned parts are not indications for escharotomy, but cyanosis, impaired capillary refilling, and signs of neurologic dysfunction, such as relentless deep tissue pain and progressive paresthesia, are. Should evidence of vascular impairment be present, escharotomy should be promptly performed. The procedure can be carried out in the ward or emergency room without anesthesia, since it is performed through insensate full-thickness burn. An initial escharotomy incision is placed in the midlateral line of the involved extremity and, if this does not improve distal blood supply, a second escharotomy incision is made in the midmedial line in the longitudinal axis of the limb. The escharotomy incision should be carried throughout the entire length of full thickness burn to ensure adequate release of vascular compression. The incision must cross involved joints, since in those areas the paucity of subcutaneous tissue permits ready compression of vessels and nerves. The escharotomy incision is carried through the eschar and the immediately subjacent thin connective tissue to permit expansion of the edematous subcutaneous tissue. When performed in this manner, blood loss from the escharotomy incision is not excessive and is readily controlled by either electrocoagulation or brief application of pressure.
Fasciotomy is rarely necessary for relief of vascular compromise in a limb with conventional thermal injury. Fasciotomy may be required in patients with high voltage electric in jury, in other patients with burns involving deep tissues, or in patients with associated traumatic injuries (i.e., patients in whom edema is pre. sent below the investing fascia). Fasciotomy should be performed in the operating room using appropriate anesthesia.
Patients with circumferential truncal burns may also require escharotomies in the anterior axillary line to relieve restriction of chest wall movement by the eschar and permit a more satisfactory ventilatory exchange. This is particularly important in children with truncal burns who may be rapidly exhausted by the increased respiratory effort required. These patients frequently will be restless, agitated, and hypoxemic before escharotomy and will show prompt clinical improvement as well as improved ventilatory exchange and blood oxygenation following escharotomy. An incision along the lower margin of the rib cage may be necessary in those patients with deep burns extending onto the upper abdominal wall (Figure 16).