TABLE OF CONTENTS
INTRODUCTION
1 DISEASES/DISORDERS OF THE GENITALIA
Section I. Diseases/Disorders of the Male Genitalia
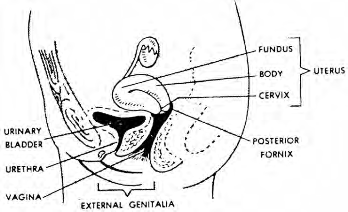
Section II. Diseases/Disorders of the Female
Genitalia
Exercises
2 SEXUALLY TRANSMITTED DISEASES
Section I. General Information
Section II. Specific Types of Sexually Transmitted
Diseases
Section III. Laboratory Texts and Procedures
Section IV. The Contact Interview
Exercises
3 HUMAN IMMUNODEFICIENCY VIRUS (HIV) AND ACQUIRED
IMMUNE DEFICIENCY SYNDROME (AIDS)
Exercises
4 DIURETICS
Exercises
------------------------------------------
LESSON 1
DISEASES/DISORDERS OF THE GENITALIA
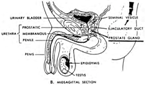
Section I. DISEASES/DISORDERS OF THE MALE GENITALIA
1-1. INTRODUCTION
Diseases and disorders of the genitalia can be
dangerous. Such problems are generally agreeable to therapy if the
diagnosis can be established. In your later work, you may be assessing
and treating these types of diseases and disorders almost on a daily
basis.
1-2. PROSTATITIS
The condition prostatitis is an inflammation of the
prostate gland. Prostatitis can be divided into two main categories:
(1) acute and chronic bacterial prostatitis and (2) nonbacterial
prostatitis. The incidence of prostatitis increases with age.
a. Etiology. Bacterial
prostatitis is either acute or chronic and is usually caused by
gram-negative organisms such as these: Escherichia coli (most common),
Enterobacter, Serratia, Klebsiella, and Pseudomonas. The causative
bacterial may reach the prostate gland from the blood stream or from
the urethra. Prostatitis is commonly associated with urethritis or an
infection of the lower genitourinary tract (an infection such as
gonorrhea). Systemic dehydration can play an important part in
decreased urinary output. This decreased urinary out put allows
microorganisms in the genitourinary tract to multiply.
b. Signs and Symptoms.
Included are the following:
(1) Burning on urination.
(2) Pain in the perineum,
rectum, lower back and abdomen, glans of the penis.
(3) Chills and moderate to
high fever.
(4) Dysuria, polyuria,
hematuria.
(5) Urethritis.
(6) Urethral discharge (clear
viscous to milk white discharge).
(7) Prostate enlarged, boggy,
and very tender.
NOTE: In the condition chronic
prostatitis, there may be no symptoms.
c. Treatment. Follow
these steps.
(1) Bed rest.
(2) Balanced fluid intake.
(3) Drug therapy. Included are
the following:
(a) Analgesic drugs for pain.
(b) Trimethoprim (80 mg) twice
a day for 30 days OR
(c) Sulfamethoxazole (400 mg)
twice a day for 30 days.
(d) For sulfa sensitive
patients:
1 Gentamicin sulfate (Garamycin®).
2 Ampicillin (Polycillin®).
(4) Culture and sensitivity
test of urine. This test can determine the specific drug that will
combat the infection.
NOTE: Treatment will depend on
the type of prostatitis present--acute or chronic bacterial
prostatitis or nonbacterial prostatitis.
(5) Neither the patient nor
the physician should massage or milk the penis.
d. Special Considerations.
(1) Be sure the patient
understands that bed rest and adequate hydration are necessary. He may
need stool softeners and sitz baths, as ordered by the doctor.
(2) Be sure the patient knows
that he must take the prescribed drugs faithfully.
(3) It is important for him to
know that he must drink at least eight glasses of water a day.
(4) Tell the patient to report
immediately signs of possible adverse reaction to drugs, signs such as
rash, nausea, vomiting, fever, chills, and gastrointestinal
irritation.
From The
Genitourinary System II